More Facts About Achilles Tendonitis:
The Achilles tendon does not have a rich blood supply. Blood supply is weakest at a point between 2 and 6 cm above its insertion into the calcaneus (heel bone).
Ignoring pain in the Achilles tendon (ie. "running through the pain") is the biggest cause of chronic Achilles tendonitis.
For cyclists, initial Achilles tendon stress is often caused by having a low saddle height. This low saddle height can result in excessive dorsiflexion of the foot, which stresses the Achilles tendon.
The Achilles tendon is the connection between the heel and the most powerful muscle group in the body.
Tennis and soccer players over 40 are the most frequent sufferers of tennis leg (calf muscle strain).
Sudden increases in running and or active sprinting sports can cause Achilles tendonitis.
Excessive running up and down hills can aggravate the Achilles tendon.
Stiff shoe soles at the ball of the foot will increase Achilles tendon strain.
Excessive heel shock absorption can overstretch the Achilles tendon.
Tight hamstrings and/or tight calf muscles create excess strain on the Achilles tendon.
For triatheletes, the most common cause of injuries to the Achilles tendon is overpronation, inflexibility, or lack of strength.
Immobility, due to an Achilles injury, may result in a contracted Achilles tendon and an increased amount of scar tissue.
| Back of Heel Pain
Pain at the back of the heel is termed "posterior heel pain". Most posterior heel pain happens due to overuse, poor fitting shoes or sandals or from overtraining. If you are experiencing pain at the bottom of the heel, the cause is most likely plantar fasciitis.
So, What Is Causing My Posterior Heel Pain
If you are experiencing pain at the back of your heel that is not due to a skin injury (such as a blister) or a bone injury (chipped bone or fracture) then it is almost certain that you are suffering from achilles tendinitis, bursitis or referred pain.
Causes of Posterior Heel Pain - Achilles Tendinitis
Tendinitis can be classified in two categories - acute tendinitis or chronic tendinitis. Acute tendinitis means you have experienced a recent injury in which your achilles tendon has become strained or partially torn. Chronic tendinitis means that you have had this condition for a lengthy period of time. A chronic case occurs when the Achilles tendon becomes inflamed over a period of time. This is often due to repetitive overuse, irritation or may be a result of acute tendinitis that has been left untreated or has not been allowed sufficient rest. It is common that the tendon becomes enlarged and inflexible due to the buildup of scar tissue.
 Acute Achilles tendinitis is typically the result of an injury or specific event that caused a strain or tearing of the Achilles tendon. When the fibers of a tendon are torn, they become inflamed and swollen causing pain and tenderness in the area which can also result in difficulty flexing the foot during regular movements, such as walking and jumping.
Most commonly, this condition is seen in athletes who sit at a desk all week and then plays softball or tennis on the weekend. The aftereffect is tendon strain (mild tears) creates inflammation and pain and can lead to tendinitis. This condition could also be created if the tendon is strained from a sudden trauma such as a fall or misstep.
Achilles tendinitis can occur at the insertion point of the tendon (referred to as insertional tendinitis) at the calcaneus (heel bone) or mid way up the Achilles tendon (referred to as non-insertional tendinitis or "achilles tendinitis a the midpoint"). The most common area to be affected by acute tendinitis is approximately 1/3 of the way up the tendon, 2.5 inches from where it attaches to the heel bone. This part of the Achilles tendon is at most risk of tendinitis and other tendon injuries because it receives less blood flow than other parts of the tendon.
Acute Achilles Tendinitis: Symptoms
If you are suffering from Acute Achilles Tendinitis you will most likely be experiencing:
- Pain that occurs abruptly following a tendon strain, usually part way up the Achilles tendon.
- Sharp pain at the beginning of activity that decreases in intensity as exercise progresses.
- Pain that returns after exercise or after long periods of inactivity.
- Pain may subside when the Achilles tendon is allowed to rest.
- Pain becomes most significant when pushing off or jumping.
- Stiffness in your Achilles tendon when you wake up in the morning.
- Tender and warm to the touch.
- The Achilles tendon is irritated by heat but feels good when treated with cold compression and rest.
Chronic Achilles Tendinitis: Symptoms
- A gradual onset of pain with no specific event known as the cause
- A thicker or swollen Achilles tendon
- Constant pain throughout exercise and even during daily activity
- A possible lump in the tendon approximately 2 inches above the heel
- Pain that increases when walking uphill or up stairs
- Pain and stiffness after long periods of rest
- Tender and warm to the touch
- Pain becomes most significant when pushing off or jumping
- A creaking feeling may occur when you press the tendon or move your ankle
If you feel a sharp pain, as though you've been hit in the back of the ankle, and hear a "pop" sound, your Achilles tendon has likely ruptured. A ruptured (completely torn) Achilles tendon can occur when the Achilles tendon is overstressed to the point of tearing. It will be very difficult for you to walk or move your ankle if this is the case.
Acute Achilles Tendinitis: Causes
Acute Achilles tendonitis may be caused by:
- Improper stretching before and after running and jumping exercises.
- Changes in foot wear (i.e. high heels, poor running shoes).
- An inflexible Achilles tendon (i.e. tendon with scar tissue from previous injury or wear and tear).
- An increase in training, training on uneven terrain or a change in terrain (i.e. hills).
- Weak or inflexible calf muscles (gastrocnemius or soleus muscles).
Achilles tendinitis is one of those injuries that can really bring down the quality of your life. Anyone - young or old - can suffer from this injury, and if you're active this condition will keep you from doing the things you love to do. It will even start interrupting any of your normal daily tasks and make living life harder than it really needs to be.
Chronic Achilles Tendinitis: Causes
- Acute Achilles tendinitis that has gone untreated.
- Not warming up or stretching before and after exercise.
- Wearing high heels over a long period of time. High heels cause the calf muscles to shorten (contract) providing less slack in the Achilles tendon.
- An inflexible Achilles tendon (i.e. tendon with scar tissue from previous injury or wear and tear or acute Achilles tendinitis).
- Training on uneven terrain or a change in terrain (i.e. hills) .
- Weak or inflexible calf muscles (gastrocnemius or soleus).
- Flat feet (also called pes planus or fallen arches) can cause extra stress on the Achilles tendon.
- Overpronation of the foot (rolling your foot inward too much when you walk or run which may be due to having high arches).
- Bony growths around the heel (sometimes caused by arthritis) which irritate the Achilles tendon.
- Heel bones can very in shape and size from person to person. With such variations, a small heel bone can put extra stress on your Achilles tendon causing you to more of a chance of damage then the next person. An irregular shape calcaneus (heel bone) can cause the Achilles tendon to twist causing further irritation.
Chronic Achilles tendinitis can be a difficult condition to treat due to the build up of scar tissue on the tendon. Scar tissue can form in any direction. Ultimately what causes stiffening, entrapping a nerve, restricting movement, less elasticity, poor circulation, flexibility and leaves the tendon more chance to further injury.
Achilles Tendinitis: Treatment
Your doctor will prescribe a series of conservative treatment protocols for you to follow. In most cases, a conservative treatment protocol will be enough to heal the injury, though in cases such as significant tearing or a fully ruptured tendon, you will most probably require surgery. It is generally understood by doctors and surgeons, that surgery will introduce more scar tissue into the any already damaged tissue. This added scar tissue will be problematic, requiring more PT and conservative treatment options post-surgery. If not dealt with properly, your Achilles tendon injury could end up in worse condition than before the surgery! This is why surgery is only performed as a last resort.
Some conservative treatment methods recommended include:
- Rest - This is important for initial recovery for both Midpoint and Insertional Achilles Tendonitis; rest and elevation will help reduce pain, swelling and inflammation in the early stages of injury. This can be difficult when you have to carry on with daily activities, but resting and elevating your foot whenever you can is recommended. During your recovery you will probably have to modify or avoid the activities that put stress on your Achilles tendon until your pain and inflammation settles. Too much rest can also be harmful to achilles injuries because ankle joint immobility can actually cause stiffening in the joint. This is why rest should be used when reducing initial pain and swelling, but should not be considered for more long-term conservative treatment.
 - Avoid Activities that Caused Your Injury - While resting your injury it's also important to avoid all activities that may have caused your tissue damage (especially any repetitive movement). Continuing on with regular activities can increase the severity of your injury, turning a mild to moderate case of tendon damage into a downward spiral of worsening damage that may eventually severely impact your life. Also, trying to 'work around' your injury will eventually give rise to over-compensation injuries in other areas of your body.
- Use a Cold Compress or Ice Pack - Cold is very effective at reducing pain and inflammation - use at the onset of the injury and during flareups.
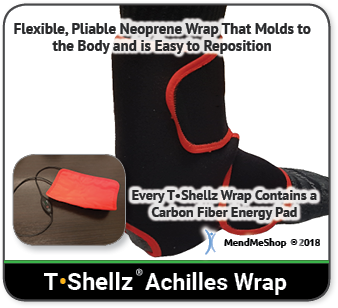
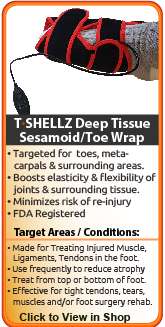
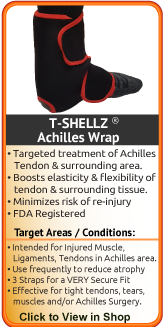
- Use an Achilles TShellz Wrap® (Circulatory Boost device) Once The Swelling is Down - You can use your own blood flow to maximize your rehabilitation, maintain healthy blood flow to your achilles and heel, decrease recovery time, reduce re-injury risk, and boost the bodys' healing rate. Promoting blood flow to the injury using a warming treatment will help to minimize the growth of scar tissue and increase flexibility. This is why we recommend TShellz Wrap before undergoing activity - an increase in flexibility should help reduce risk of further injury while also assisting in the battle against atrophy.
- Use an Achilles Support Wrap - to increase comfort and prevent further damage you may want to use a ankle support sleeve or brace to help support the area, reduce risk of further injury and reduce stress on the injured tissue. Some of these are also designed for heat retention to prevent further strain. They can be used until your injury is gone or during active sports for additional stability. Note that these should not be worn at all times, as they can limit muscle development, cut off circulation and impede healing of muscle tissue.
- Avoid Over Compensating for your Injury on your "'Healthy' (Non-Injured) Side - Many people will start limping or carrying objects with their opposite arm to compensate for their tendon injury. Our bodies can adapt easily to any changes, including a tendonitis injury. This quick adaptation could mean that you're already compensating for your injury without even knowing it!
When you compensate for your injury by using your opposite ('healthy') arm, leg, shoulder, knee, foot, etc. - then you are putting more weight and pressure on that side of your body. In many cases, your dominant side was injured (if you're right-handed this would be your right side) so your weaker side is trying to pick up the slack! The pain, stiffness, swelling and inflammation you then get on your 'healthy' side is something referred to as 'over-compensation pain'. Over-compensating for your injury can lead to other injuries and so that's why over compensation should be avoided at all costs OR treated with the same conservative treatment methods as your tendon injury.
- Rehabilitative Stretching under supervision of a PT or doctor. The intent of this is to provide you with increased range of motion, pain relief and strengthening of the surrounding tissue of the joint. Doctors or surgeons typically won't perform a surgery until they feel that their patient has put effort into treating their injury with conservative treatment methods. This may include up to 4 to 6 months of visits to a PT clinic. If you haven't experienced any improvement in your condition during that time then surgery may be considered. Agressive PT approaches may focus on forced or manual manipulation of the achilles - this means your physical therapists will be trying to move your achilles past the point of comfort as they strive to increase range of motion and prevent further atrophy. This can be painful and end up making your injury worse if not done correctly. (reference: 1)
- Stretching - Stretching your joint in PT and at home will help you to regain your range of motion much faster than not stretching at all. Stretching in many ways is key maintaining good Range of Motion (ROM) in your joint, and stretching can be made much easier with use of a TShellz Wrap® before to warm up soft tissue, and a Cold Compress or Ice Pack treatment after to prevent any return of swelling and inflammation.
Read more about conservative treatment options for achilles tendonitis by clicking here.
Causes of Posterior Heel Pain - Achilles Bursitis
A bursa is a sac of synovial fluid, rich in protein and collagen, that lies between a tendon and a bone to help the tendon glide smoothly over the bone. There are 2 bursae that surround the Achilles tendon to protect it from friction. The retrocalcaneal bursa lies between the tendon and the back, or posterior surface, of the heel bone (calcaneus). This is a "true" bursa that is present from birth. It acts as a cushion between these two structures to protect the tendon from friction against the heel bone.
The larger subcutaneous calcaneal bursa lies overtop of the tendon at the lower part of the heel where the tendon joins to the heel bone. This bursa develops as you age, an "adventitious" bursa, to protect the tendon from friction at the back of the heel.
Bursitis occurs when a bursa is irritated from frequent pressure and it becomes inflamed. When one or both of these bursa become inflamed it is generally referred to as Achilles bursitis because of the bursa's proximity to the Achilles tendon. In some cases, an inflamed bursa can become infected with bacteria (referred to as septic bursitis) and it is necessary to see a doctor to get rid of the infection.
Due to the proximity to the area on the Achilles tendon, Achilles bursitis is often mistaken for tendinitis. Achilles bursitis is a common overuse injury in runners, ice skaters and other athletes.
Achilles Bursitis: Symptoms
When you suffer from Achilles bursitis it will be most noticeable when you begin an activity after rest:
 - Pain at the back of the heel, especially with jumping, hopping, tip-toeing, walking or running uphill or on soft surfaces. If tendonitis is also present, the pain can radiate away from the bursa.
- Direct pressure on the bursa will exacerbate the pain and should be avoided if possible.
- Tenderness and swelling which might make it difficult to wear certain shoes on the feet.
- As the bursa becomes more inflamed you will experience swelling and warmth. In severe cases, the bursa will appear as a bump, called a "pump bump", and is usually red, and extremely tender. Swelling can cause difficulties moving as the range of motion in the ankle can be affected.
- Limping due to the pain may occur
- If you press on both sides of the inflamed heel, there may be a firm spongy feeling.
- Weakness in the tendons and muscles surrounding the bursa can develop as the pain worsens and the inflammation in the area spreads.
- Possibly a fever if you are suffering from septic bursitis (You will need to see a doctor for medication to get rid of the infection).
- For individuals who wear high-heeled shoes frequently, they may also feel an increase in pain when they are wearing flat shoes. When wearing high-heels, the calf muscles and Achilles tendon remain in a shortened position. When flat shoes are worn it causes the calf muscles and Achilles tendon to stretch more than usual causing the tendon to tighten around the heel bone causing irritation.
Achilles Bursitis: Causes
- Tight shoes or shoes that do not fit properly can cause extra pressure on the back of the heel.
- Athletes overtraining or runners increasing their distance to quickly.
- Haglund deformity, a bony enlargement on the back of the heel bone, during dorsiflexion causes an impingement of the bursa between the Achilles tendon and the heel bone.
Achilles Bursitis: Treatments
Relieving the symptoms of bursitis initially focuses on taking the pressure off the bursa. This can be done with proper cushioning, inserts, or footwear but may require surgery if it is a bone formation problem (i.e. Haglund's Deformity). If your bursitis is caused by an infection (septic bursitis), the doctor will probably drain the bursa sac with a needle and perscribe antibiotics to treat the infection.
For non-infectious bursitis, the preliminary treatment starts with conservative treatment options. Such options typically include cold compression and Circulation Boost. Surgery to remove the inflamed bursa is normally not required for bursitis, however if you fail to see improvement with the conservative treatments, your physician may recommend surgery to remove the bursa completely. Although this removes the problem of an inflamed bursa, you are left with less cushioning in your joint which can lead to other conditions such as fraying of the tendons, muscles or ligaments in the treated area. Eventually, fraying can lead to increasing weakness and rupture in severe cases.
Read more about conservative treatment options for achilles bursitis by clicking here.
Causes of Posterior Heel Pain - Referred Pain at Back of Heel
Referred pain is the strangest issue to get your head around and it is not exactly a common issue, but can manifest itself via an irritation of the spinal nerve between the fifth lumbar and the first sacral vertebrae. In cases such as referred pain, it goes without saying that you should see a physician to get a proper diagnosis as well as proper treatment. In such instance, a proper treatment may include some back treatments, recommendations for change in posture, anti-inflammatory medications and PT.
Learn More About Achilles Injuries & TreatmentsI want to learn more about Achilles Surgery & Post-Surgery Recovery I want to learn more about Circulation Boost I want to learn more about Ice & Heat: Which Is Better For The Achilles? I want to learn more about Stretching for the Achilles
FREE SHIPPING ON ALL PRODUCTS CURRENTLY ENABLED
60 DAY TRIAL PERIOD
During your recovery, you will probably have to modify and/or eliminate any activities that cause pain or discomfort at the location of your soft tissue injury until the pain and inflammation settle. The more diligent you are with your treatment and rehabilitation, the faster you will see successful results!
|

Achilles Tendon Facts
There are over 250,000 achilles tendon injuries each year in the US.
Achilles tendon ruptures are common in people between the ages of 30 and 50.
In runners, too rapid an increase in mileage, hill training without proper strengthening, and recent or inadequate changes to running gear can cause injuries to the Achilles tendon.
Achilles tendonitis accounts for an estimated 11% of running injuries.
3-5% of athletes are forced to leave their sports career due to Achilles tendon overuse injuries that go untreated.
Medications mask the pain but do very little in the healing of Achilles tendonitis.
A fully ruptured tendon REQUIRES surgery. It will not heal on its own.
Achilles tendonitis and Achilles tendinitis are the same thing.
Continually using your Achilles tendon while it is injured will lead to a more serious and/or chronic injury.





|